Discover essential insights into diabetic foot care with our authoritative guide. Learn about prevention, symptoms, and innovative treatments to maintain your foot health and enhance your quality of life.
Introduction
Welcome to our comprehensive guide on managing diabetic foot, a common yet often preventable complication of diabetes. This condition, stemming from neuropathy (nerve damage) and poor circulation, can lead to severe foot problems if not addressed promptly. Our article delves into the causes, symptoms, and cutting-edge treatments for diabetic foot, empowering you with knowledge to protect your feet and sustain your mobility and well-being.
Table of Contents
Understanding Diabetic Foot

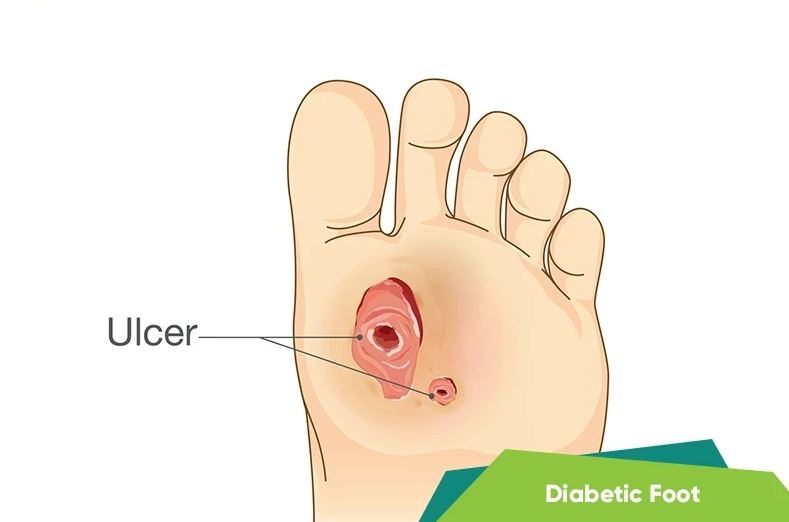
Diabetic foot refers to a range of foot problems that can occur in individuals with diabetes. These issues often stem from two main complications of diabetes: neuropathy (nerve damage) and poor circulation. Understanding these causes, recognizing the symptoms, and implementing effective prevention strategies are key to managing diabetic foot and maintaining overall foot health.
Causes of Diabetic Foot
Neuropathy (Nerve Damage): Diabetes can cause nerve damage over time, leading to a loss of sensation in the feet. This numbness means injuries, sores, or infections might go unnoticed, increasing the risk of complications.
Poor Circulation: Diabetes can affect blood flow, making it harder for blood to reach the extremities, like the feet. Poor circulation slows down the healing process of any cuts or wounds, heightening the risk of infections or ulcers.
Symptoms to Watch For

Numbness or Reduced Sensation: One of the earliest signs of diabetic foot is a lack of feeling in the feet or toes.
Tingling or Pain: A burning sensation or sharp pains in the feet can indicate nerve damage.
Changes in Skin Color: A change in the color of the feet, such as becoming more red, blue, or pale, can signal circulation problems.
Swelling: Swelling in the feet or ankles might indicate underlying issues related to diabetic foot.
Sores or Ulcers That Don’t Heal: Slow-healing wounds are a significant concern and can lead to more severe infections.
Infections: Any signs of infection, such as warmth, redness, or discharge, require immediate medical attention.
The Importance of Regular Foot Examinations for Diabetics
Regular foot examinations play a pivotal role in the early detection and management of diabetic foot issues, serving as a critical component in the prevention of severe complications such as ulcers, infections, and even amputation. For individuals with diabetes, both self-examinations at home and professional check-ups are essential practices that can significantly impact their overall foot health and quality of life.
Self-Examinations at Home
Self-examinations should be a daily routine for anyone with diabetes. These simple checks can help identify potential problems early, when they are easier to treat. Here’s how to perform a thorough self-examination:
Inspect Your Feet Daily: Look for any cuts, sores, blisters, redness, calluses, or ingrown toenails. Use a mirror to check the bottoms of your feet or ask someone to help if you’re unable to see them clearly.
Feel Your Feet: Use your hands to feel for any lumps, bumps, or swelling. Check for temperature differences between your feet, which could indicate circulation issues.
Check for Changes: Notice any changes in the color or shape of your feet, as these can be early signs of problems.
Monitor Pain or Sensation Changes: Be aware of any new pain, tingling, numbness, or other sensations. These could be signs of neuropathy or circulation issues.
Professional Check-Ups
While self-examinations are crucial, professional foot check-ups provide an additional layer of protection. These should be scheduled at least once a year, or more frequently if recommended by your healthcare provider. During a professional examination, you can expect:
Comprehensive Foot Inspection: Your healthcare provider will look for any of the signs you check for at home, with the added benefit of their professional expertise to catch subtler signs of trouble.
Neurological Examination: Tests may be performed to check the nerves in your feet, often using a monofilament to test sensitivity to touch.
Vascular Assessment: Your doctor will check the blood flow to your feet, looking for any signs of poor circulation.
Skin and Nail Care: Professionals can safely manage calluses, corns, and toenails, preventing complications that could arise from attempting to treat these issues at home.
Footwear Assessment: Your healthcare provider can recommend the right type of shoes and socks to wear, helping to prevent pressure sores and blisters.
The Significance of Early Intervention
Early detection through regular foot examinations is key to preventing the progression of diabetic foot issues. Identifying and treating minor problems before they develop into serious complications can save your feet and potentially your life. Regular monitoring and maintenance can prevent infections, ulcers, and the need for hospitalization or surgery.
Innovative Treatments and Solutions for Diabetic Foot Complications

The management of diabetic foot complications has seen significant advancements in recent years, with innovative treatments and solutions improving outcomes for patients. These developments range from cutting-edge wound care technologies to surgical interventions, alongside the integration of custom orthotics and lifestyle modifications. Together, these approaches offer a comprehensive strategy for preventing and managing diabetic foot problems.
Cutting-Edge Wound Care Technologies
Advanced Dressings: Modern wound dressings, such as those containing silver or honey, offer antimicrobial properties, promoting faster healing and reducing the risk of infection.
Growth Factor Therapy: This involves applying growth factors directly to the wound to stimulate healing. Growth factors are proteins that play a crucial role in the body’s repair processes.
Skin Substitutes: Bioengineered skin substitutes can be used to cover large ulcers, providing a temporary or permanent solution to help wounds heal when traditional methods have failed.
Negative Pressure Wound Therapy (NPWT): Also known as vacuum-assisted closure, NPWT uses suction to draw out fluid from the wound and increase blood flow to the area, accelerating healing.
Surgical Interventions
For severe cases of diabetic foot, surgical options may be necessary:
Debridement: The removal of dead or infected tissue to improve the healing potential of the remaining healthy tissue.
Revascularization: Procedures to restore blood flow to the affected area, such as angioplasty or bypass surgery, can be critical for patients with poor circulation.
Amputation: In extreme cases, partial or total amputation of a foot or lower leg may be necessary. However, the goal of modern diabetic foot care is to prevent amputation whenever possible through early intervention and comprehensive treatment.
Custom Orthotics and Footwear
Custom orthotics play a vital role in preventing and managing diabetic foot complications by redistributing pressure away from high-risk areas. They are designed to fit the unique contours of the patient’s feet, reducing the risk of ulcers and calluses. Specialized diabetic footwear also helps protect the feet from injury and improves comfort.
Lifestyle and Dietary Changes
Lifestyle and dietary modifications are foundational to managing diabetes and, by extension, preventing diabetic foot complications:
Regular Exercise: Physical activity improves blood circulation and can help control blood sugar levels, reducing the risk of nerve damage and poor circulation.
Healthy Diet: A diet rich in fruits, vegetables, whole grains, and lean proteins can help manage blood sugar levels, while reducing saturated fats and refined sugars supports overall vascular health.
Smoking Cessation: Smoking exacerbates circulation problems, making it more difficult for wounds to heal. Quitting smoking is crucial for individuals with diabetes.
Blood Sugar Management: Keeping blood sugar levels within target ranges is essential to prevent the long-term complications of diabetes, including those affecting the feet.
The integration of these innovative treatments and solutions, combined with a commitment to lifestyle and dietary changes, offers hope and improved quality of life for individuals dealing with diabetic foot complications. As research continues, further advancements are expected, enhancing the ability to manage and prevent these serious health issues effectively.
Footwear Tips for People with Diabetes: Protecting Your Feet

For individuals living with diabetes, selecting the right footwear is not just about comfort or style—it’s a crucial aspect of managing their health and preventing serious foot complications. Poorly fitting shoes can lead to blisters, sores, and ulcers, which, in the context of diabetes, can lead to severe infections due to compromised blood flow and nerve damage. Here are essential footwear tips for people with diabetes to protect their feet and maintain their mobility and quality of life.
1. Choose the Right Fit
Get Professionally Measured: Foot size and shape can change over time, especially with diabetes. Get your feet measured professionally to ensure you’re buying the right size.
Account for Swelling: Feet can swell during the day. Try on shoes in the afternoon or evening when your feet are at their largest.
Width Matters: Make sure the shoes are wide enough. Shoes that are too narrow can cause pressure points, leading to blisters and calluses.
2. Look for Supportive Features
Good Arch Support: Proper arch support can distribute pressure evenly across your feet, reducing the risk of pain and injury.
Cushioning: Look for shoes with cushioning to absorb impact and protect your feet.
Adjustable Closure: Shoes with laces, buckles, or Velcro straps can be adjusted for a snug, comfortable fit, accommodating changes in foot size due to swelling.
3. Opt for Breathable Materials
Breathable Fabrics: Shoes made from leather, canvas, or other breathable materials can help keep your feet dry and reduce the risk of fungal infections.
Moisture-wicking Linings: Some shoes come with moisture-wicking linings to draw sweat away from your feet, keeping them dry and comfortable.
4. Minimize Seams and Check for Smooth Interiors
Seamless or Smooth Interiors: Rough seams and materials inside the shoe can rub against your skin, leading to blisters or sores. Choose shoes with minimal internal seams or those lined with soft, smooth materials.
5. Consider Specialized Diabetic Shoes and Custom Orthotics
Diabetic Shoes: These are specially designed to reduce the risk of skin breakdown in people with diabetes who are at risk for foot complications. They often feature extra depth to accommodate orthotics.
Custom Orthotics: Custom-made shoe inserts prescribed by a healthcare provider can correct specific foot issues, distribute pressure evenly, and prevent complications.
6. Regularly Inspect and Replace Footwear
Inspect Shoes Regularly: Check for any signs of wear and tear, such as holes, worn soles, or interior seams that may cause irritation.
Replace When Necessary: Don’t wait for shoes to fall apart before replacing them. Worn-out shoes lose their supportive and protective features.
7. Avoid Going Barefoot
Protect Your Feet Always: Even at home, wear shoes or slippers to protect your feet from cuts, scratches, and infections.
FAQ Section
Q: What is diabetic foot? A: Diabetic foot refers to foot problems that occur due to diabetes-related complications like neuropathy and poor circulation, leading to infections, ulcers, and potentially severe outcomes.
Q: What are the symptoms of diabetic foot? A: Symptoms include numbness, tingling, pain, changes in skin color, swelling, and slow-healing sores or ulcers.
Q: How can I prevent diabetic foot complications? A: Prevention strategies include regular foot examinations, proper footwear, managing blood sugar levels, and adopting a healthy lifestyle.
Q: What treatments are available for diabetic foot complications? A: Treatments range from advanced wound care technologies and surgical interventions to custom orthotics and lifestyle modifications.
Q: Why is regular foot examination important for diabetics? A: Regular foot examinations help in early detection and management of potential foot problems, preventing serious complications.
Conclusion
Managing diabetic foot requires a proactive approach focused on prevention, early detection, and innovative treatment strategies. By understanding the risks and adopting comprehensive care practices, individuals with diabetes can significantly reduce the likelihood of complications. Embrace the journey towards healthier feet with the insights and strategies outlined in our guide, ensuring a better quality of life and mobility.
Remember, maintaining healthy feet as a diabetic doesn’t just improve your quality of life—it could very well save it. Stay informed, stay vigilant, and let’s walk towards a healthier future together.